Please wait...

Please wait...
Our team will work with you to review all of your treatment options and choose the treatment that best suits your needs and goals. Our treatment philosophy is based on a multimodality approach. This means that we customarily explore more than one form of therapy to treat liver tumors.
(Open Surgery)
Our team of doctors may recommend traditional open liver surgery, depending on the size and location of the tumors. Resection of a large portion of the liver is possible because the remaining liver grows to compensate for the part that was removed. The best chance for successful treatment of liver cancer is with surgery. If all of the cancer can be removed, the possibility of successful treatment is higher. Surgery to remove part of the liver is called liver resection or partial hepatectomy.
(Laparoscopic Liver Surgery)
Our team of doctors at the Liver Cancer Center may recommend minimally invasive liver surgery -also called laparoscopic surgery – over traditional surgery, based on the location and size of the tumors. In minimally invasive procedures, your doctor makes one or more incisions, each about a half-inch long, to insert a tube. The tube or tubes let the doctor slip in tiny video cameras and specially designed surgical instruments to perform the procedure. When you have minimally invasive surgery, you’re likely to lose less blood and have less postoperative pain, fewer and smaller scars, and a faster recovery than you would after open surgery. Depending on your condition, you may need only a short hospital stay. As leaders in minimally invasive (laparoscopic) surgical liver resection, our surgeons can remove certain benign or malignant liver tumors through three or four keyhole – sized incisions.
(Open Surgery)
Our team of doctors may recommend traditional open liver surgery, depending on the size and location of the tumors. Resection of a large portion of the liver is possible because the remaining liver grows to compensate for the part that was removed. The best chance for successful treatment of liver cancer is with surgery. If all of the cancer can be removed, the possibility of successful treatment is higher. Surgery to remove part of the liver is called liver resection or partial hepatectomy.
(Laparoscopic Liver Surgery)
Our team of doctors at the Liver Cancer Center may recommend minimally invasive liver surgery -also called laparoscopic surgery – over traditional surgery, based on the location and size of the tumors. In minimally invasive procedures, your doctor makes one or more incisions, each about a half-inch long, to insert a tube. The tube or tubes let the doctor slip in tiny video cameras and specially designed surgical instruments to perform the procedure. When you have minimally invasive surgery, you’re likely to lose less blood and have less postoperative pain, fewer and smaller scars, and a faster recovery than you would after open surgery. Depending on your condition, you may need only a short hospital stay. As leaders in minimally invasive (laparoscopic) surgical liver resection, our surgeons can remove certain benign or malignant liver tumors through three or four keyhole – sized incisions.
Liver transplantation may be the best option for some people with small liver cancers. At this time, liver transplants are reserved for those with small tumors (either 1 tumor smaller than 5 cm or 2 to 3 tumors no larger than 3 cm) that have not invaded nearby blood vessels. This criteria is called Milan Criteria. In most cases, transplant is used for tumors that cannot be totally removed, either because of the location of the tumors or because the liver is too diseased (cirrhotic) for the patient to withstand removing part of it. The 5-year survival rate for these patients is around 65% to 70%. Most livers for transplants come from people who have just passed away (brain dead). This is known as Cadaveric Liver Transplantation or Disease Donor Liver Transplantation (DDLT). The other option is to have a Living Donor Liver Transplantation where a family donor donates a part of liver to the cancer patient. The liver has a capacity to regenerate if a part of it is removed. The donated part of the liver and the remaining liver in the donor regenerates in two to three months.
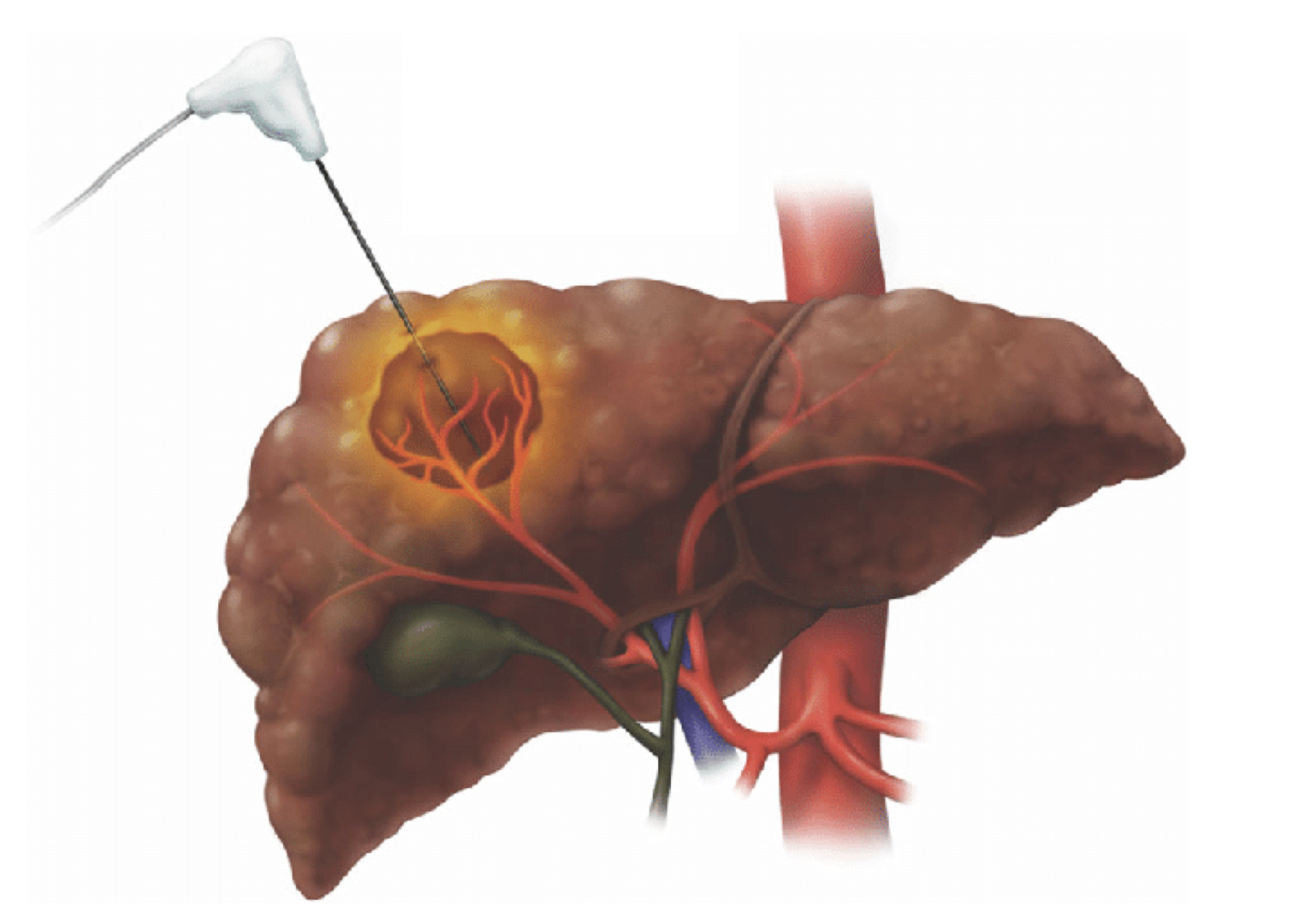
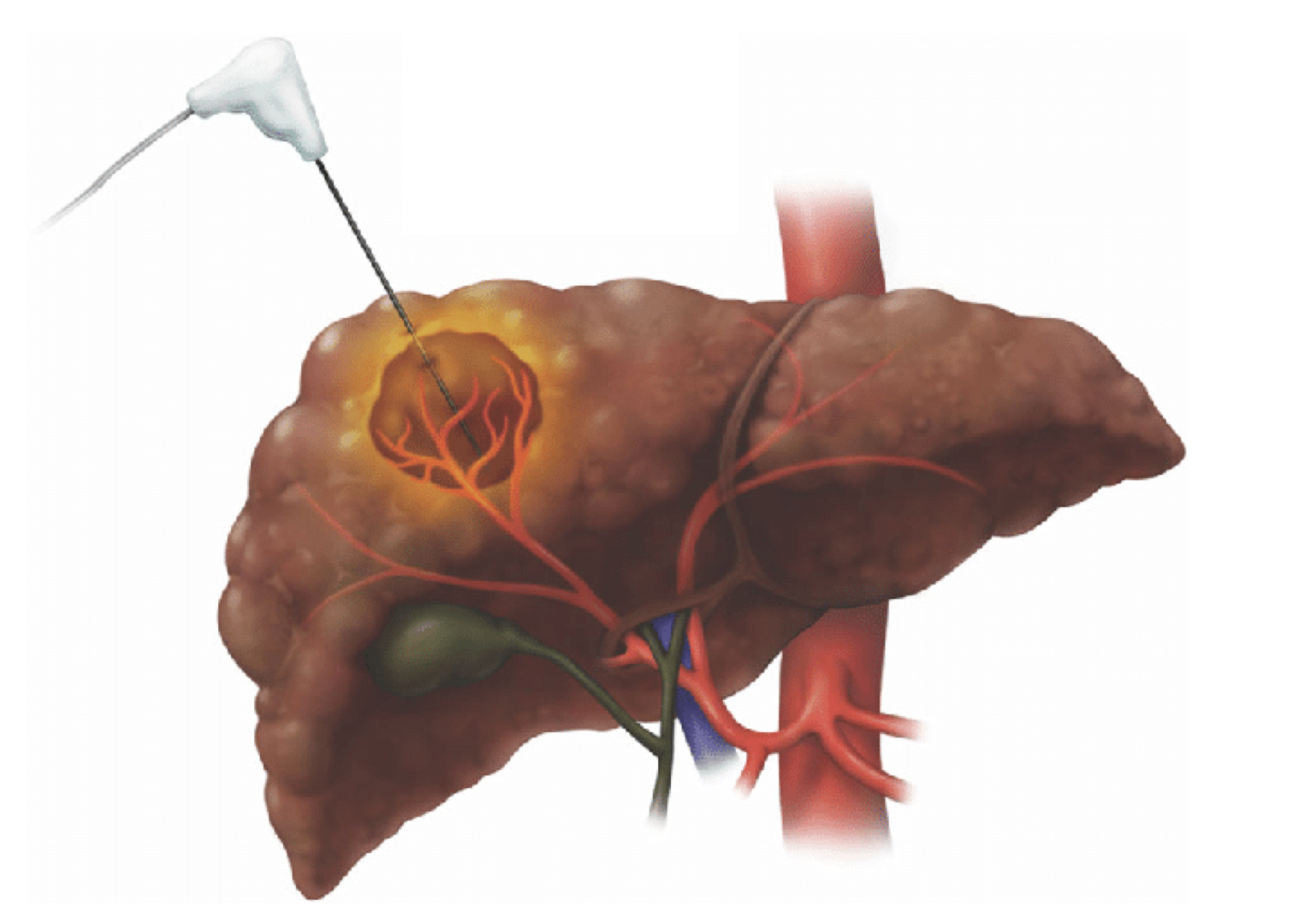
Radiofrequency ablation (RFA) is one of several types of ablation therapy when surgery for certain types of cancer is not a good option. It is a minimally invasive treatment. Guided by imaging techniques, the doctor inserts a thin needle through the skin and into the tumor. High-frequency electrical energy delivered through this needle heats and destroys the tumor. Months after the procedure, dead cells turn into a harmless scar. Whether you are a good candidate for RFA depends on several issues, such as the size and location of your tumor. In most cases, only a single RFA treatment is necessary for any given tumor. The RFA technique appears to be best for tumors less than 5 centimeters in size.
Liver transplantation may be the best option for some people with small liver cancers. At this time, liver transplants are reserved for those with small tumors (either 1 tumor smaller than 5 cm or 2 to 3 tumors no larger than 3 cm) that have not invaded nearby blood vessels. This criteria is called Milan Criteria. In most cases, transplant is used for tumors that cannot be totally removed, either because of the location of the tumors or because the liver is too diseased (cirrhotic) for the patient to withstand removing part of it. The 5-year survival rate for these patients is around 65% to 70%. Most livers for transplants come from people who have just passed away (brain dead). This is known as Cadaveric Liver Transplantation or Disease Donor Liver Transplantation (DDLT). The other option is to have a Living Donor Liver Transplantation where a family donor donates a part of liver to the cancer patient. The liver has a capacity to regenerate if a part of it is removed. The donated part of the liver and the remaining liver in the donor regenerates in two to three months.
Radiofrequency ablation (RFA) is one of several types of ablation therapy when surgery for certain types of cancer is not a good option. It is a minimally invasive treatment. Guided by imaging techniques, the doctor inserts a thin needle through the skin and into the tumor. High-frequency electrical energy delivered through this needle heats and destroys the tumor. Months after the procedure, dead cells turn into a harmless scar. Whether you are a good candidate for RFA depends on several issues, such as the size and location of your tumor. In most cases, only a single RFA treatment is necessary for any given tumor. The RFA technique appears to be best for tumors less than 5 centimeters in size.
Trans-arterial chemoembolization (or TACE) combines embolization with chemotherapy. In this procedure a catheter is put into an artery through a small puncture in the inner thigh under local anesthesia and threaded up into the hepatic artery in the liver. A dye is usually injected into the bloodstream at this time to help the doctor monitor the path of the catheter via angiography, a special type of x-ray. Once the catheter is in place, the chemotherapy drug is directly injected into the artery. With this technique, the chemotherapy targets the tumor while sparing the patient many side effects of traditional chemotherapy that is given to the whole body. Following chemotherapy, our interventional radiologist will embolize (cut off) the blood supply to the tumors. In this manner, the tumor is treated using two different techniques. If necessary, TACE can be performed multiple times to achieve the desired response in the tumor. This type of treatment requires one-day hospital stay.
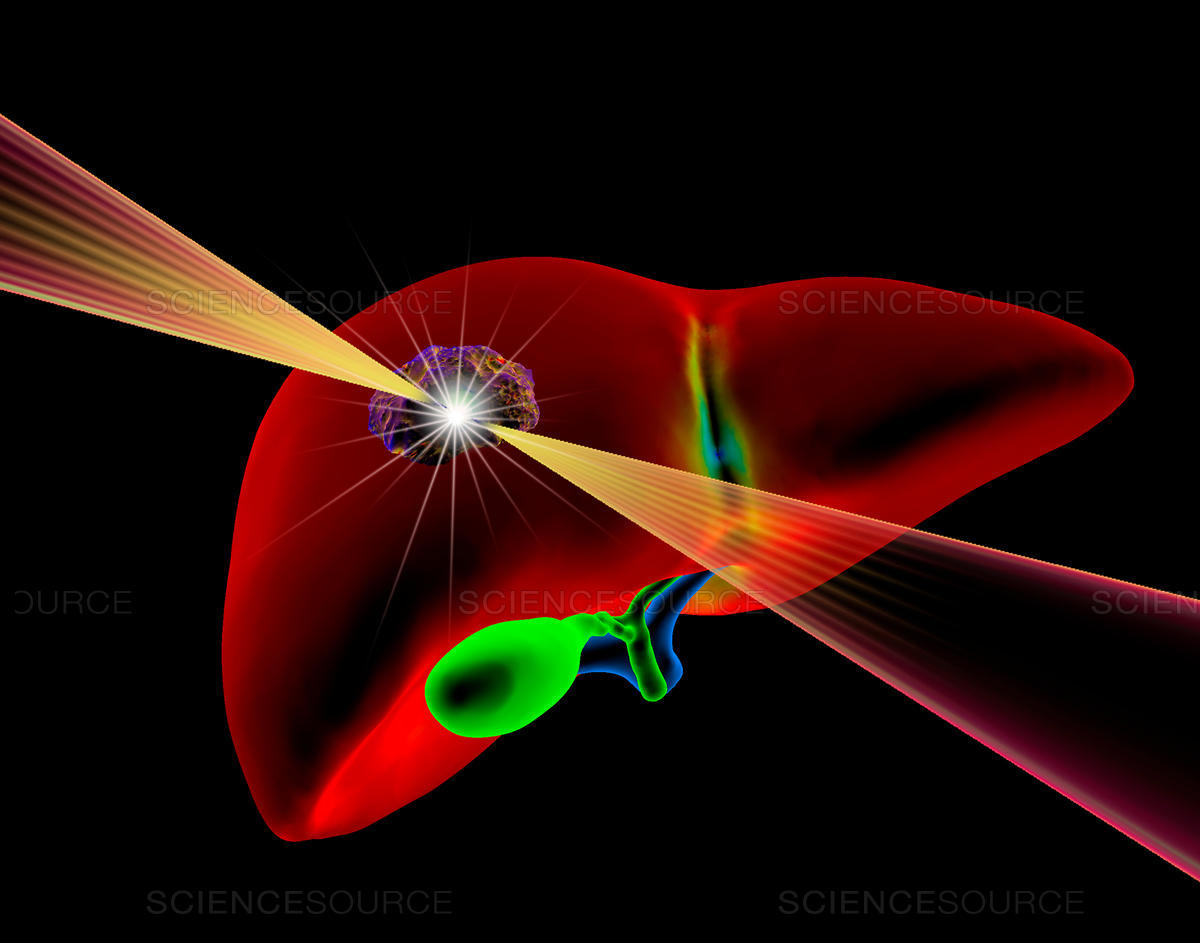
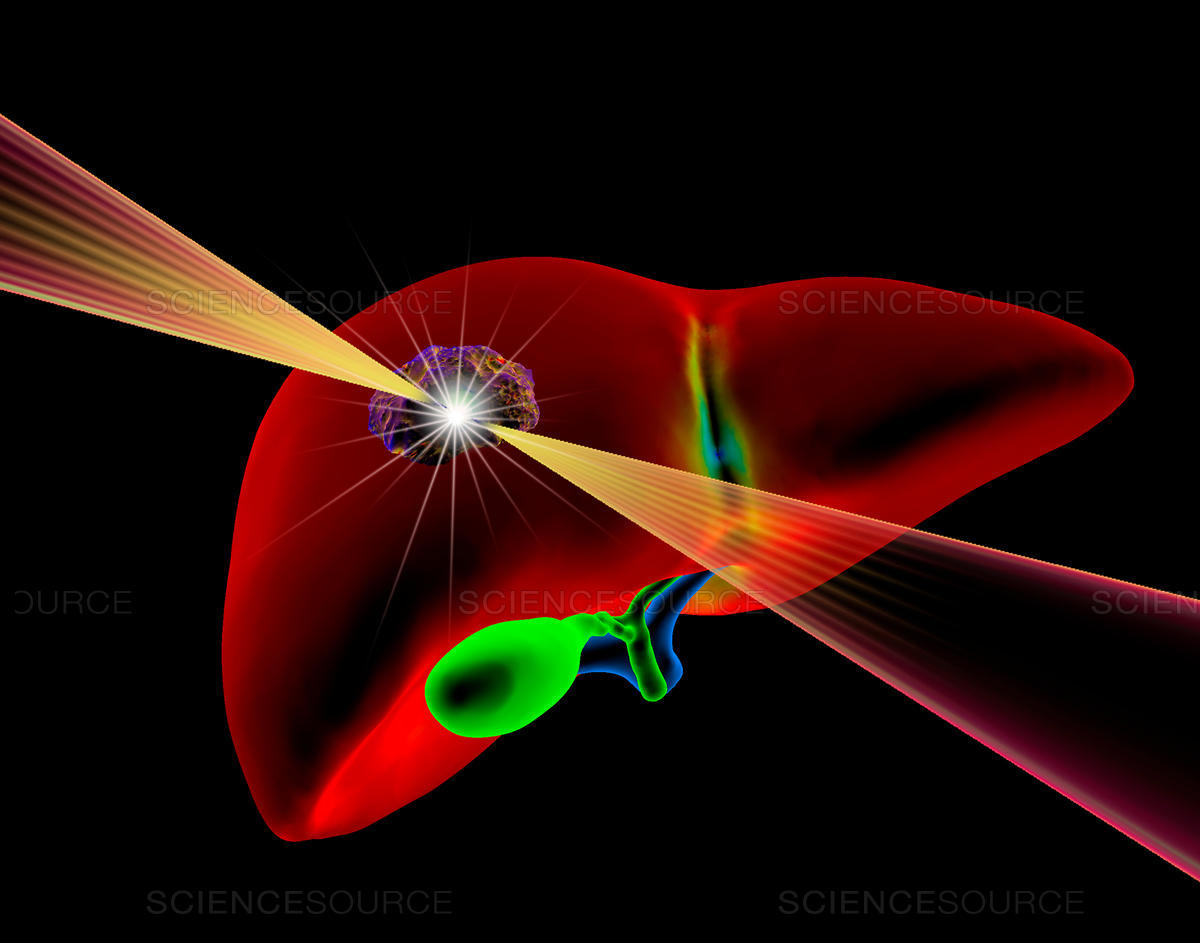
Radioembolization (Yttrium-90) is very similar to chemoembolization but with the use of radioactive microspheres. This is a newer and innovative technique combines embolization with radiation therapy. This is done by injecting small radioactive glass-beads (called microspheres) into the hepatic artery. This therapy is used to treat unresectable (inoperable) liver cancer, and cancers that metastasize to the liver from other parts of the body, such as the colon, lungs, breast or pancreas. This treatment is frequently used in patients with multiple liver tumors. Radioembolization is a palliative, not a curative, treatment-but patients benefit by extending their lives and improving their quality of life.
Trans-arterial chemoembolization (or TACE) combines embolization with chemotherapy. In this procedure a catheter is put into an artery through a small puncture in the inner thigh under local anesthesia and threaded up into the hepatic artery in the liver. A dye is usually injected into the bloodstream at this time to help the doctor monitor the path of the catheter via angiography, a special type of x-ray. Once the catheter is in place, the chemotherapy drug is directly injected into the artery. With this technique, the chemotherapy targets the tumor while sparing the patient many side effects of traditional chemotherapy that is given to the whole body. Following chemotherapy, our interventional radiologist will embolize (cut off) the blood supply to the tumors. In this manner, the tumor is treated using two different techniques. If necessary, TACE can be performed multiple times to achieve the desired response in the tumor. This type of treatment requires one-day hospital stay.
Radioembolization (Yttrium-90) is very similar to chemoembolization but with the use of radioactive microspheres. This is a newer and innovative technique combines embolization with radiation therapy. This is done by injecting small radioactive glass-beads (called microspheres) into the hepatic artery. This therapy is used to treat unresectable (inoperable) liver cancer, and cancers that metastasize to the liver from other parts of the body, such as the colon, lungs, breast or pancreas. This treatment is frequently used in patients with multiple liver tumors. Radioembolization is a palliative, not a curative, treatment-but patients benefit by extending their lives and improving their quality of life.
A new technology, microwave ablation (MWA), destroys liver tumors using heat generated by microwave energy. With microwave ablation, the surgeon inserts a small laparoscopic port or open incision to access the tumor. A CT scan or ultrasonic guidance is used to pinpoint the exact location of the tumor. A thin probe, which emits microwaves, is then inserted into the tumor. The probe produces intense heat that ablates (destroys) tumor tissue, often within 10 minutes.
A new technology, microwave ablation (MWA), destroys liver tumors using heat generated by microwave energy. With microwave ablation, the surgeon inserts a small laparoscopic port or open incision to access the tumor. A CT scan or ultrasonic guidance is used to pinpoint the exact location of the tumor. A thin probe, which emits microwaves, is then inserted into the tumor. The probe produces intense heat that ablates (destroys) tumor tissue, often within 10 minutes.